Prescription Notes Auditing in a Medical College and Hospital of Himachal Pradesh - Juniper Publishers
JUNIPER PUBLISHERS-GLOBAL JOURNAL OF PHARMACY & PHARMACEUTICAL SCIENCES
Authored by Kansal D
Abstract
Introduction: Prescription audit is necessary to know the prescription practices and to improve rational pharmacotherapy. In India few publications are available on prescription audit.
Materials and method: This was an observational study, undertaken between August 2016 to October 2016 for which data was collected from our OPDs. Results were compiled, tabulated and analyzed using Microsoft excel. Charts were drawn to present all the findings.
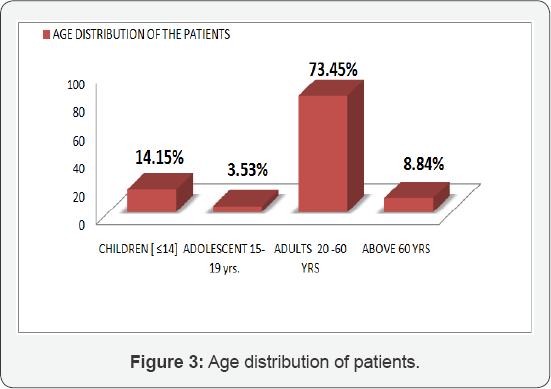
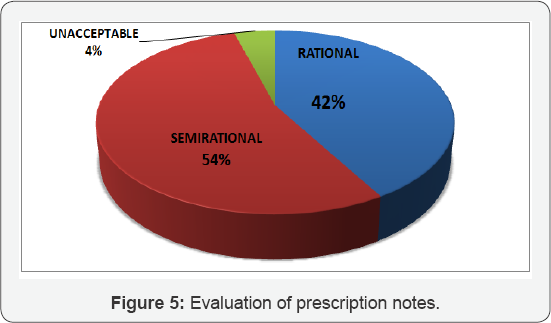
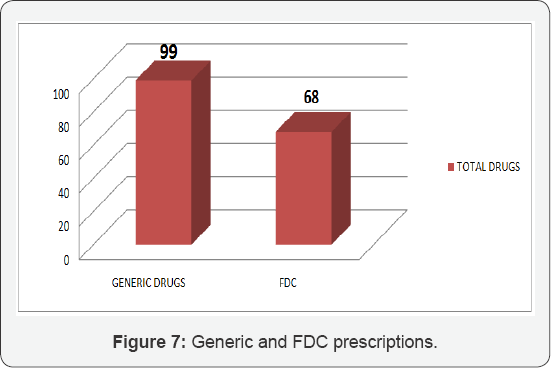
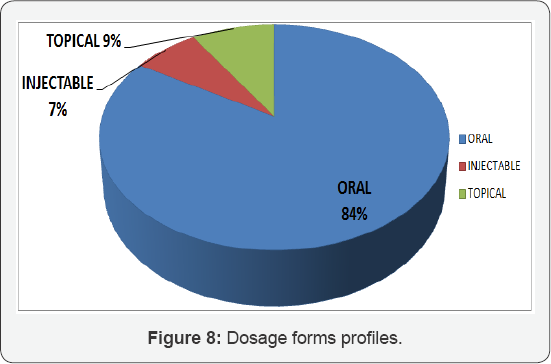
Results: In total 317 medications were prescribed in 113 prescription notes. Therefore average number of drugs/prescription was 2.80. Demographic profile shows more females (58.40%) as compared to males (41.60%). Maximum patients (73.45%) were from adult age group, followed by children (14.15%). Most common dosage form was oral in 83.59%, topical were prescribed in 9.14% and injectable were recommended in 7.25%. Drugs were prescribed by generic name in 31.23% and as fixed dose combinations in 21.45%. Complete diagnosis was written in 63.71%. Findings were written in 60.17%. Signatures were done in 92.92%. Only 78.76% prescriptions were complete in terms of dose, route, frequency and duration. Advice was written only in 41.59% of prescriptions. On evaluation 54% prescriptions were semi rational (Scoring between14-18), 41.59% were rational (scoring between 20-24) and 4.42% were unacceptable (scoring less than 12).
Conclusion: Our study showed that there is scope for improvement in prescribing patterns in areas of writing of complete prescriptions in respect of diagnosis, signature, advise, dose, frequency and duration.
Keywords: Prescription auditing; Drug utilization pattern; Rational pharmacotherapy
Introduction
With prescription audit the main aim is to improve rational use of drugs. Irrational prescriptions can lead to adverse drugs reactions or sub therapeutic treatment and antimicrobial resistance. Irrational prescribing is a universal problem. Examples include: poly pharmacy, inadequate dosage, use of antimicrobials even for non-bacterial infections and excessive use of injections when oral forms are available [1].
The World Health Organization (WHO) has formulated a set of "core prescribing indicators" for improvement in rational drug use in outpatient practice. It includes the prescribing indicators, the patient care indicators and the facility indicators [2]. Based on these indicators, studies have been carried out all over the world and even in India [3].
Aim and objectives
o We will analyze the prescriptions under these subheadings.
o Department wise distribution of the patients.
o Demographic profile of population i.e. male female ratio and age-distribution.
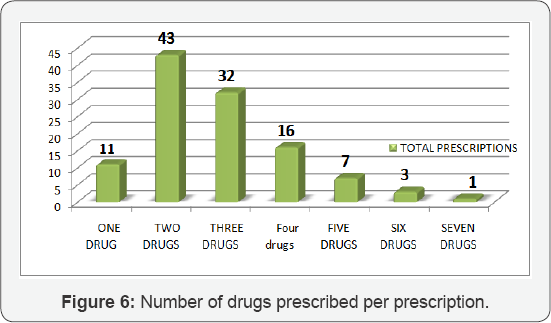
o Number of drugs per prescription.
o Completeness of diagnosis, findings, signatures, dose, frequency and duration of treatment.
o Drug dosage forms; oral/injectable/topical.
o Evaluation of prescription as Rational (score 20-24), Semi Rational (score 14-18) and Unacceptable (score less than 12).
Material and Methodology
This was an observational, prospective study carried out over a period of 3 month between August to October 2016. The data was collected from OPDs of our hospital. These prescriptions were analyzed based on the objective of the study. Complete information i.e. specialty wise distribution, age, sex, demographic profile of patients, prescription profile and number of drugs per prescription. These were uploaded on M.S. Excel sheet. These results were analyzed and deficiencies were observed.
Evaluation of prescriptions was done by twelve questions. Each carries 2 marks so total marks were 24.
These twelve questions were:
a) Completeness of Prescription:
I. Diagnosis
II. Findings
III. Signature
b) Whether prescription corroborates with symptoms/ Diagnosis
IV. Selection of core drugs
V. Selection of symptomatic drug
VI. Relevant advices for patients
c) Prescribing behavior:
VII. Generic prescription
VIII. Essential drugs prescription
IX. Judicious investigations
d) Dosage schedule:
X. Dose
XI. Frequency
XII. Duration of therapy
Evaluation scheme
Total marks 24 (100%)
Marks obtained 18 to 24 = Rational.
Marks obtained 12 to 18= Semi rational.
Marks obtained <12 = unacceptable.
Results
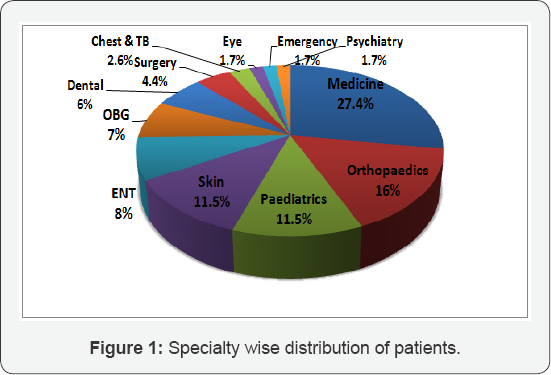
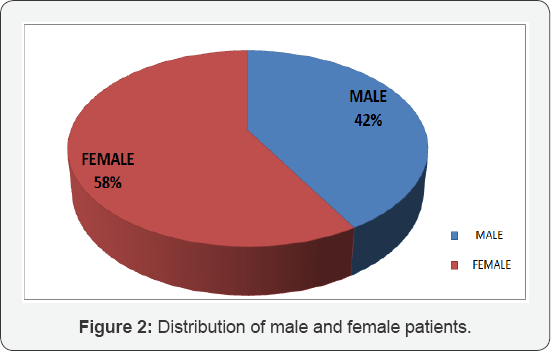
In total 317 drugs were prescribed in 113 prescriptions. So average number of drugs/prescription were 2.80 drugs.Specialty wise distribution shows that 27.4% patients were from Medicine, 16% were from Orthopedics, 11.5% each were from Pediatrics and skin and rest 33.6% patients were from ENT, OBG, Dental, Surgery, Chest and TB, Eye, Emergency medicine and Psychiatry (Figure 1). Demographic data (Figure 2) shows female 58% and male 42%. 73.5% of patients were in the 20-60 years age group (Figure 3). Findings were written in 68(60%) prescriptions. Diagnosis was complete in 72(64%) patients. Advices were written in 47(41.59%) prescriptions. And 89(79%) of prescriptions notes were complete in dose/ frequency and duration. Signatures were done in 105(93%) prescriptions (Figure 4).
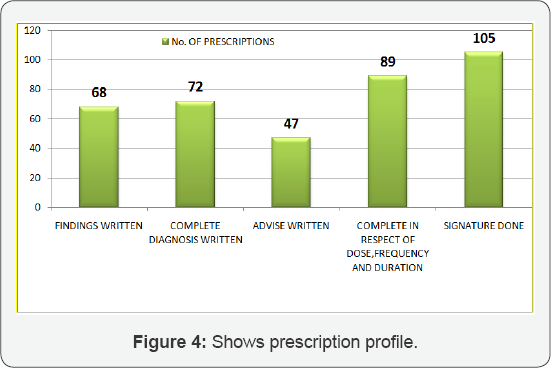
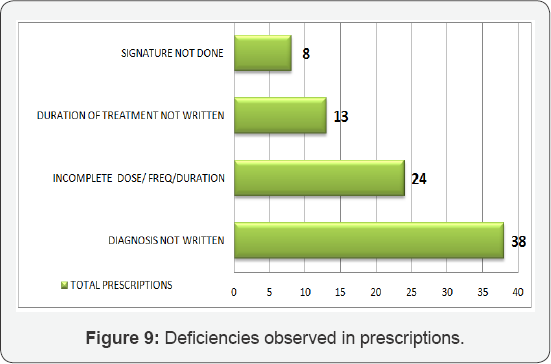
Evaluation of these prescription was done as rational (score 20-24), semi rational (14-18) and unacceptable (score less than 12). Result of these prescriptions were maximum of semi rational 61(54%), rational 47(42%) and unacceptable 5(4%) (Figure 5). 75 prescriptions contained 2-3 drugs. In only 27 prescriptions more than 3 drugs were prescribed (Figure 6). Drugs prescribed by generic names were 99(31.23%) and drugs prescribed as FDC were 68(21.45%) (Figure 7). Most commonly oral drugs were prescribed (84%) followed by topical in (9%) and least were injectable (7%) (Figure 8). Deficiencies observed in prescriptions were diagnosis not written in 38 prescription notes (33.62%), incomplete either in dose, frequency or duration 24(21.23%), Duration of treatment was not written in 13 (11.50%) and signature was not done in 8 prescription notes (7.07%) (Figure 9).
Discussion
Prescription auditing is an important tool to improve rational pharmacotherapy. It is very important document for health administrators and clinicians groups for both decision making and drafting policies. In our study total drugs prescribed were 317 in 113 prescription notes. Therefore average numbers of drugs/prescriptions were 2.80. So result was quite satisfactory to the recommended limit of 2.0 [2]. This limit is to prevent drug- drug interactions and unwanted side effects. FDCs were used in 21 % of prescriptions. This figure is also quite low compared to two indian studies which reported 75% and 60 % usage of FDCs respectively [4-10]. FDCs sometimes may be irrational. Our study also show Poly pharmacy. 52% of prescriptions shows either 3 or more than 3 drugs. Even this poly pharmacy is a big concern and it is reported in various studies [5,9].
In 84% prescriptions oral formulation, in 9% topical and in 7% prescriptions injectable were prescribed. Although use of injectable was high from other studies but it was at par with Indian study which reported 7% [3]. We need further decrease in number of injectable, to reduced blood born infections [6]. In our study antibiotics were prescribed in 18.3% of cases. More than one antibiotics was prescribed in 7% of cases. Results were satisfactory and are much lower than other study [7] in which around 50% of patients received more than one antibiotic. Overuse of antibiotics leads to drug resistance.
In 31% of prescriptions generic drugs were prescribed. This is very low as compared to other studies, few study reported very high (73.4%) use of generic names [8]. Generic prescribing decreasing the chances of dispensing errors. Lot of deficiencies were observed in prescription writing like diagnosis not written in 38(34%), signature not done in 8(7%), and duration of treatment not written in 13(11.50%) of prescription notes. Around 24(21.23%) of prescriptions were incomplete either in dose/ frequency or duration. So there was a scope for improvements in the prescription writing.
Conclusion
From our study it is concluded that there is scope for improvement in prescribing patterns in areas of writing diagnosis, findings, signature, advise, dose, frequency and duration. Educating the clinicians about prescription writing is very important aspect. Regular updates of clinicians are also required for improving rational pharmacotherapeutics.
For more articles in Global Journal of Pharmacy & Pharmaceutical Sciences please click on https://juniperpublishers.com/gjpps/index.php
For more about Juniper Publishers please click on https://juniperpublishers.com/index.php



Comments
Post a Comment